Comprehensive Analysis of Ivermectin
Scientific Evidence, Regulatory Decisions, and Controversies
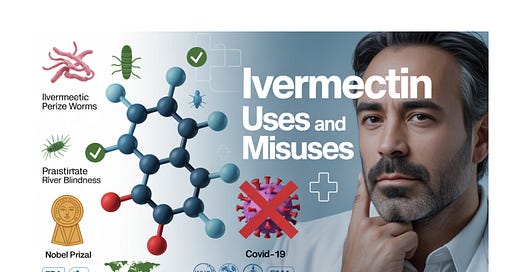
Ivermectin is a Nobel Prize-winning antiparasitic drug with proven efficacy against specific parasitic infections, but current evidence does not support its use for COVID-19. Early promising COVID-19 studies were largely compromised by poor methodology and potential fraud, while high-quality recent trials consistently show no benefit. Manufacturing costs are extremely low (approximately $0.12 per course), but regulatory barriers and quality concerns have shaped access patterns globally.
1. Discovery and Historical Context
Nobel Prize-Winning Origins
Ivermectin's discovery earned William Campbell and Satoshi Ōmura the 2015 Nobel Prize in Physiology or Medicine for "their discoveries concerning a novel therapy against infections caused by roundworm parasites." The drug was first discovered in 1975, initially for veterinary use, and approved for human use in 1987.
The discovery originated from a unique Public-Private partnership in the early 1970s between Satoshi Ōmura at Tokyo's Kitasato Institute and Merck Sharp and Dohme (MSD). In 1970, Ōmura isolated a strain of Streptomyces avermitilis from woodland soil near a golf course along the southeast coast of Honshu, Japan.
Development Process
At Merck, William Campbell led research that discovered one compound from the bacterial cultures was remarkably effective against parasites in farm animals. The bioactive agent was purified and named Avermectin, which was subsequently chemically modified to create Ivermectin.
2. Established Medical Uses and Efficacy
Proven Therapeutic Applications
Ivermectin is approved to treat infestations including head lice, scabies, river blindness (onchocerciasis), strongyloidiasis, trichuriasis, ascariasis and lymphatic filariasis. It is on the World Health Organization's List of Essential Medicines.
Global Health Impact
Thanks to ivermectin, river blindness has been essentially eliminated in 11 Latin American countries, preventing approximately 600,000 cases of blindness. Since the inception of the Mectizan Donation Programme, Merck has donated well over 2.5 billion Mectizan® tablets for Onchocerciasis treatment, with in excess of 700 million treatments authorized. Currently, some 80–90 million people are taking the drug annually through mass drug administration in Africa, Latin America and Yemen.